Cards In This Set
| Front | Back |
|
Describe and identify the DRG cell ending types and the sensory modalities transduced by each type.
|
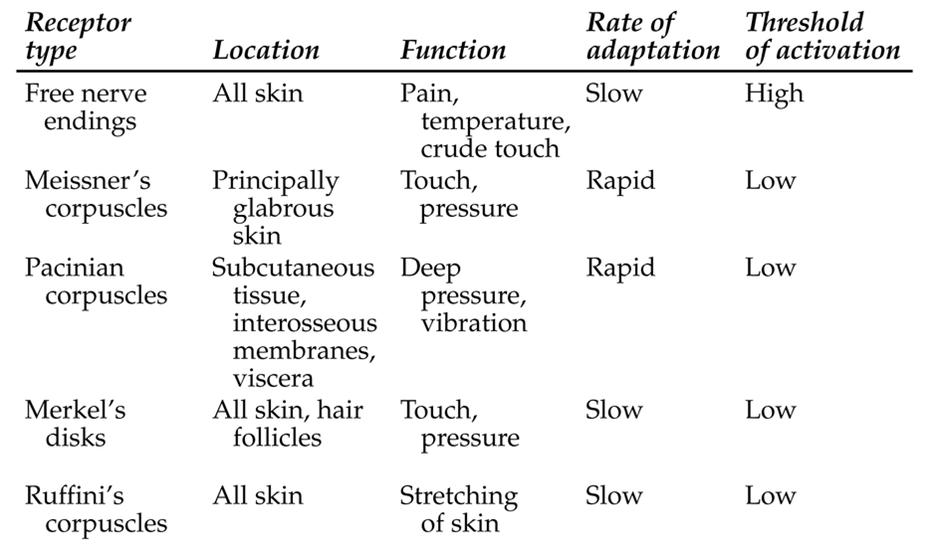 Only very end of dorsal route ganglia has cell body |
|
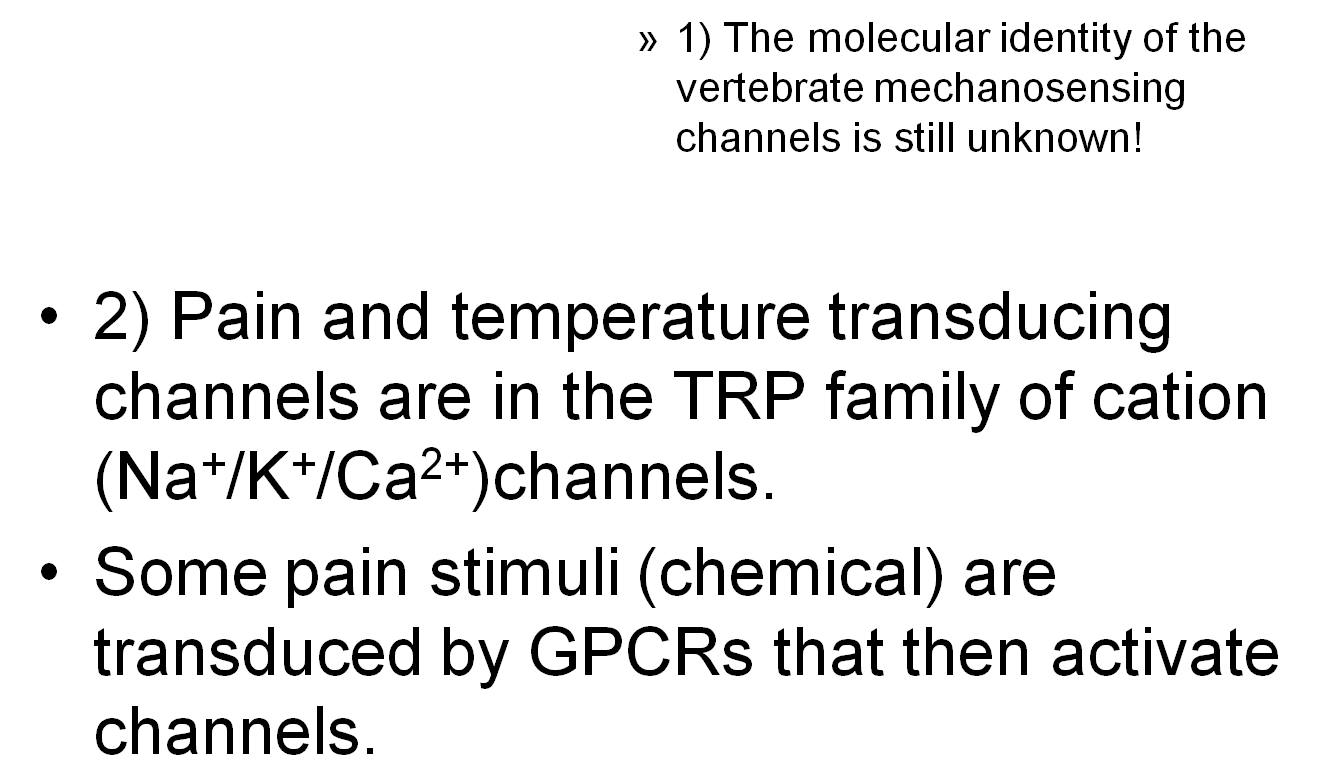
What are ion channels that transduce sensory modalities? how do we know that mechanosensing channels are cation that open upon membrane displacement
|
 *you can record the ion flow thru the open channels with a voltage clamp as a bar applies pressure to the cell, and categorize as SA, IA, or RA |
|
Describe and understand the difference between SA and RA currents and relate them to different physiological properties of DRGs
|
*RA DRG peaks then rapidly gets smaller as it adapts to the pressure stimulus. will only respond well to a "first touch"
*SA DRG is opposite, the current remains constant as long as a pressure stimulus is applied. *IA DRG is in between **** at initial stimuli, ALL THESE FIRE AT ONCE. SA's will just last longer than IA, which lasts longer than RA |
|
Describe the physiology of TRP channels and how they transduce temperature and pain info what other channels are involved in pain transduction
|
*Discovered by adding DNA coding for different channels with calcium sensitive dyes
*adding menthol (cold) or capsaicin( warm) signaled calcium flow, meaning that these TRP channels respond to temp -permeable to Ca and Na, blocked by La * 4 subunits, 6 membrane spanning regions -different types of channels have optimal temp ranges ***NOCICEPTORS also transduce pain, plus burning hot and cold temperatures |
|
Describe the location in the spinal cord and brain for the first 4 synapses for somatosensation and pain
|
1. DRG to spinal column
2. spinal column to thalamus 3. thalamus to somatosensory cortex 4. |
|
Describe where pain/temp and somatosensory pathways diverge to be transmitted ipsilaterally and contralaterally. describe how unilateral spinal cord damage effects pain/temp and somatosensation differently
|
The mechanosensory pathway travels ipsilaterally (same side) and doesn't synapse until it gets to brain stem
*pain cells travel contralaterally, and cross over after their first synapse in the spinal column to the other side * with spinal chord damage, touch and pain sensation would be preserved on opposite sides |
|
Describe a specific parallel map and an orthoganol map in the primary somatosensory cortex
|
READ
|
|
Describe how phantom limb sensations and pain relate to cortical maps, and how mirror box therapy indicates a "top down" effect on sensory cortical maps.
|
When you lose input coming up from DRG, part of your brain won't have any S.S input
* phantom limb is caused by that area of the brain whose cells are still active *areas that are nearby start picking up information from area that doesnt have input -i.e for phantom limb, arm maps onto face |
|
Describe and name the descending pathways that modify pain sensation through endogenous opiates
|
*gated by 2 pathways, both interneurons
1. dorsal horn neurons gray matter: gates pain by inhibiting release neurotransmitter that very first DRG releases to transduce pain 2. periaqueductal gray matter |
|
Describe the pathways and major receptors responsible for itch sensation
|
1. histamine pathway: histamine and TRPV1 GCPRs
-activated by histamine (released from inflammatory mast cells) 2. histamine independent pathway: CQ and TRPA1 GCPR's - activated by mrgprA3 *pathway similar as pain (contralateral) - Spinal Thalamic Tract neurons in Dorsal Spinal column fire when stimulated by gastrin releasing peptide *** chronic morphine users experience chronic itch because morphine can activate a morphine receptor that's associated with a GRPR receptor |
|
What TRP channels open to menthol and what open to capsaican
|
*menthol: TRPA1(freezing cold), TRPM8 (cold)
-TRPA1 can also transduce pain *capsaican: TRPV4 (warm temp) thru TRPV1 (very very hot) |
|
What channels transduce pain
|
*P2X channels (permeable to ATP)
*TRPA1 (cold) and TRPV1 (hot) *ASIC channel (acid pain, permeable to H+) |
|
Name the different toungue papillae and describe the location of taste buds, describe how they differ in content of different taste receptor cells
|
1. circumvallate papillae: in back of tounge, high content of HCL and quinine receptors
2. foliate papillae: on the sides of the toungue 3. fungiform papillae: front/side of tongue, high content of sucrose, NaCl, and HCL receptors |
|
Describe the responses of the population of chordi-tempani axons to different tastants. what is the implication of this response pattern for both the receptor types on taste cells, and for how taste info is processed (population code or labled line)
|
Certain chorda tympani axons fire ate higher rates when exposed to certain tastants (theres 40 different axons)
*a lot of mixing with sweet and salty tastants |
|
Name the specific transduction channels and receptors in taste receptor cells for salty, sour, bitter, sweet and umami. note the unique and shared mechanisms of transduction
|
 SALT: ENaC (sodium ion channel) SOUR: PKD2L (hydrogen ion channel) SWEET: T1R2 and T1R3 (shared with umami) UMAMI: T1R1, T1R1 (shared with sweet) and TRPM5 (shared with bitter) BITTER: T2R5 , PLCB2 (activates TRPM5 channeli) and TRPM5 calcium ion channel (shared with umami and sweet) |



