Cards In This Set
| Front | Back |
|
What are unique structural characteristics of mycoplasma?
|
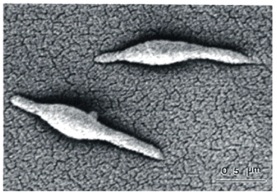 1. Tiny (smallest self-replicating organism, smallest known genome)2. No cell wall. Thus:-- Pleiomorphic: morphs between round and oblong-- Insensitive to B-lactams3. Cell membrane packed with sterols, e.g. cholesterol. (Something needs to give it structure, since there is no cell wall) |
|
What illness is caused by mycoplasma?What are the symptoms?
|
Mycoplasma causes "walking pneumonia," a mild atypical pneumonia with associated mild bronchitis. Note: Walking refers to mild symptoms - patients walk in, walk out
Symptoms [after long (2-3 week) incubation period]:fever, sore throat, malaise, persistent dry cough |
|
What are some unique laboratory characteristics of mycoplasma?
|
1. Does not Gram stain (no cell wall)2. Slow growing in (sputum) culture; 2-3 weeks. Colonies have characteristic "fried-egg" appearance.3. Require special sterol-containing medium to grow in culture (due to membrane structure).
|
|
What are virulence factors of mycoplasma?
|
Protein P1: Adhesin on mycoplasma's specialized apical structure that binds strongly to respiratory epithelium.
Note: Adhesion is a regulated process; at a given time, only 5-25% of mycoplasma are bound. Remaining bacteria are free to be released/transmitted upon coughing. |
|
How does mycoplasma evade the immune system?
|
Variation of surface antigens yields incomplete immunity.1. VLPs (variable lipoproteins): phenotypically unstable surface proteins encoded by multiple, clustered, divergent vlp genesNote: Instability due to intragenic intersertions/deletions, intergenic recombination due to sequence repeats, phase variation due to insertions/deletions in propomters)2. VSPs (variable surface lipoproteins) are also unstable (due to tandem repeats)
|
|
How is mycoplasma transmitted?
|
Respiratory droplets. At any given time, only 5-25% of mycoplasma is bound to respiratory epithelium; remainder is free to spread. Note: Highly contagious in close quarters (military barracks, college dorms, families)
|
|
How is it possible to get repeat infections of Mycoplasma pneumoniae?
|
Surface protein variability (VSPs and VLPs) means adaptive immunity is incomplete.
|
|
What is the pathophysiology of M. pneumoniae?
|
Ciliary activity is impaired -> necrosis of respiratory epithelium. Note: Mechanism unclear, maybe hydrogen peroxide
Mild inflammatory response |
|
How do we treat M. pneumoniae?
|
If infection is limited to upper respiratory tract, do not treat. If pneumonia develops, treat with macrolides, tetracyclines, quinolones (not with B-lactams - no cell wall!)
|
|
What types of Chlamydia cause atypical pneumonias?
|
C. pneumoniaeC. psittaci
|
|
Is chlamydia Gram+ or Gram-?
|
Slight trick question: Technically Gram- (two membranes, stains pink), but no peptidoglycan layer.
More importantly - chlamydia is an obligate intracellular pathogen (energy parasite that steals host ATP) |
|
What is the natural reservoir of C. psittaci?
|
Birds.
|
|
How do you grow chlamydia in culture?
|
Must be grown in human host cells; no medium to culture chlamydia has been develops.
|
|
Describe the chlamydia life cycle.
|
Cycles between two forms: EB (elementary body) and RB (replicative body)
1. Between hosts, chlamydia exists as EB. EB is a metabolically inert, fastidious small body that is stable for extracellular existence.Note: EB form is not metabollically active, thus not sensitive to inhibitors2. Once endocytosed, EB differentiates to RB form, which replicates by binary fission(using host ATP). This all occurs within endosome.Note: RB form somehow stop formation of phagolysozome 3. Secondary differentiation back to EB form, which is then exocytosed or released by cell lysis. |
|
How do we treat chlamydia? How many membranes must the drug cross?
|
Tetracycline or Erythromycin. (No peptidoglycan wall, so B-lactams won't work).
Drug must cross 4 membranes: 1. Host PM2. Vacuolar PM3. Bacterial outer membrane4. Bacterial inner membrane |



